Abstract
Background
Newly diagnosed hospitalized patients (pts) with hematologic malignancies (HM) frequently have high symptom burden, often need prolonged courses of highly myelosuppressive chemotherapy and consequent protracted transfusion support- factors that predispose these pts to unplanned readmissions (UR). Given the paucity of data on risk factors associated with repeated UR in HM pts, we first analyzed the baseline characteristics of pts with one or more 30-day UR and then evaluated factors that predicted for additional 30-day UR following the first 30-day UR event.
Methods
Adult (≥ 18 years) HM pts treated at Cleveland Clinic between January 2011-February 2016 were included in the study. Thirty-day UR was defined as hospitalization within 30 days of index admission for any reason other than planned chemotherapy. A readmission event served as an index admission for the subsequent readmission. Bone marrow transplant pts were excluded. HM included acute leukemias, myelodysplastic syndromes (MDS) and aggressive lymphomas (Diffuse Large B-Cell Lymphoma, Burkitt's). Demographics (age, race, sex, highest education attained, median income, payer status), clinical characteristics (HM type, symptoms at index admission/readmission, disease status, body mass index at discharge, absolute neutrophil count (ANC) at discharge/readmission, and discharge on intravenous antibiotics or narcotics), hospitalization (reason for readmission, length of stay (LOS) at index admission/readmission), and discharge characteristics (discharged to and readmitted from) were collected. Data were analyzed using Fisher's exact test chi-square tests, and t-tests for univariable analyses; and logistic regression for multivariable analyses. Recursive partitioning was used to find cut points for continuous factors.
Results
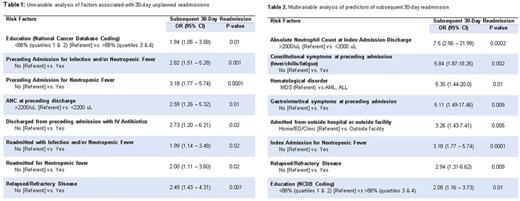
A total of 259 thirty-day UR were observed in 157 pts - 107 had a single 30-day UR, while 50 (32%) had > 2 UR. The majority of pts were males (59%), with a median age of 66 years (yrs, interquartile range (IQR) 48-75). Acute myeloid leukemia was the most common HM diagnosis (44%) and 50% had relapsed or refractory disease. Pt median income was $51,700 and 86% (IQR, 80-90%) had greater than a high school education, using census tract based data (Table 1). By payer source, 49% of pts were covered by Medicare, 12% by Medicaid, and 36% by private insurance. Discharges following UR were to: home (50%), home with home health (32%), nursing facility (15%) and hospice (3%). Of the discharges after UR, 10% were discharged on intravenous antibiotics, 44% on opioids and 48% on psychotropic drugs. Neutropenic fever with or without a confirmed source was the primary diagnosis (61%) for 30-day UR and 59% had symptoms at presentation. Median ANC at discharge from an UR was 870/mL (IQR 190-3570) and was 940/mL (IQR, 100-3700) at the time of readmission. The median LOS during 30-day UR was 5 days (IQR 3-10) and the median interval from prior discharge to readmission was 11 days (IQR 5-19). The majority of 30-day UR originated from outpatient clinic, emergency department, or pt's home (46%) followed by a non-health care facility (27%) and outside hospital transfers (22%). Table 1 shows univariable analysis of factors significantly associated with 30-day UR. In multivariate analysis, factors that independently predicted for subsequent 30-day UR included pts with the following characteristics - ANC <2000/mL at last discharge (OR 7.5, P=.0002), constitutional symptoms (fevers/chills/sweats/severe fatigue at index admission presentation) (OR 5.84, P=.002), gastrointestinal symptoms (OR 5.11, P=.009), if pt was transferred from an outside facility (OR 3.26, P=.005), febrile neutropenia as reason for index admission (OR 3.18, P=.0001), relapsed/refractory disease (OR 2.94, P=.009), and higher education (OR 2.08, P=.01).
Conclusion
Our findings suggest directing UR reduction strategies to optimize symptom control (constitutional and gastrointestinal) prior to discharge and design specific measures for the cohort with relapsed/refractory disease who might further benefit with individualized care from a multidisciplinary care team, and closer ambulatory follow up. Increased risk of additional 30-day UR with education may reflect better understanding of care complexities resulting in a lower threshold for seeking care with a change in medical condition, or possibly a surrogate for better health care access.
Gerds: Incyte: Consultancy; CTI BioPharma: Consultancy. Advani: Takeda/ Millenium: Research Funding; Pfizer: Consultancy. Sekeres: Celgene: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.